Suranjana TewariAsia Economic Correspondent, Tokyo
 BBC
BBCLast year, more than 18,000 elderly people with dementia left their homes and migrated to Japan. Nearly 500 were later found dead.
According to police, such cases have doubled since 2012.
Older people aged 65 and over now make up almost 30% of Japan’s population – the second highest proportion in the world after Monaco, according to the World Bank.
The crisis is further exacerbated by a shrinking workforce and strict restrictions on the entry of foreign workers to provide care.
The Japanese government has identified dementia as one of its most pressing policy challenges. The Ministry of Health estimates that the cost of dementia-related health and social care will reach 14 trillion yen ($90 billion; £67 billion) by 2030 – up from 9 trillion yen in 2025.
In its latest strategy, the government has signaled a greater focus on technology to ease the pressure.
Across the country, people are adopting GPS-based systems to keep track of those who wander.
Some regions offer wearable GPS tags that can alert authorities when a person leaves a certain area.
In some cities, convenience store employees receive real-time alerts, a kind of community safety net that can locate a missing person within hours.
Care robots and AI
Other technologies aim to detect dementia earlier.
Fujitsu’s aiGait uses AI to analyze posture and gait patterns and detect early signs of dementia – shuffling while walking, slower turning or difficulty standing – and generates skeletal outlines that doctors can check during routine checkups.
“Early detection of age-related diseases is crucial,” says Hidenori Fujiwara, a Fujitsu spokesman. “If doctors can use motion capture data, they can intervene earlier and help people stay active longer.”
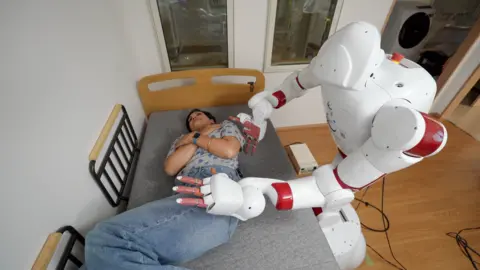
Meanwhile, researchers at Waseda University are developing AIREC, a 150kg humanoid robot designed to be a “future” caregiver.
It can help someone put on socks, make scrambled eggs, and fold laundry. Waseda University scientists hope that AIREC can change diapers and prevent bedsores in patients in the future.

Similar robots are already being used in nursing homes to play music to residents or guide them through simple stretching exercises.
They also monitor patients at night – placing them under mattresses to monitor sleep and condition – reducing the need for humans to do the rounds.
Although humanoid robots will be developed in the near future, it will take at least five years before they can safely interact with humans until they reach the required level of precision and intelligence, according to Assistant Professor Tamon Miyake.
“It requires whole-body awareness and adaptive understanding – how to adapt to each person and situation,” he says.
Emotional support is also part of the innovation push.
Poketomo, a 12cm tall robot, can be carried around in a bag or fit in a pocket. It reminds users to take medications, tells them in real time how to prepare for the weather outside, and offers conversations for those living alone, which the developers say helps alleviate social isolation.
“We focus on social problems… and using new technologies to help solve those problems,” Sharp development manager Miho Kagei told the BBC.
While devices and robots offer new ways to provide support, human connection remains irreplaceable.
“Robots should complement human caregivers, not replace them,” said Mr. Miyake, the Waseda University scientist. “Although they perform some duties, their primary role is to assist both caregivers and patients.”
People flock to the Restaurant of Mistaken Orders in Sengawa, Tokyo, founded by Akiko Kanna, to be served by patients with dementia.
Inspired by her father’s experience with the disease, Ms. Kanna wanted to create a place where people could stay engaged and feel purposeful.
Toshio Morita, one of the cafe’s waiters, uses flowers to remember which table ordered what.
Despite his cognitive decline, Mr. Morita enjoys the interaction. For his wife, the café offers peace and quiet and helps him keep busy.
Kannas Café illustrates why social interventions and community support remain essential. Technology can provide tools and relief, but meaningful engagement and human connection are what truly keep people with dementia alive.
“Honestly? I wanted some pocket money. I like meeting all kinds of people,” says Mr. Morita. “Everyone is different – that’s the fun.”
 Getty Images
Getty ImagesAdditional reporting from Jaltson is the Chammar